Category: Health Policy
-
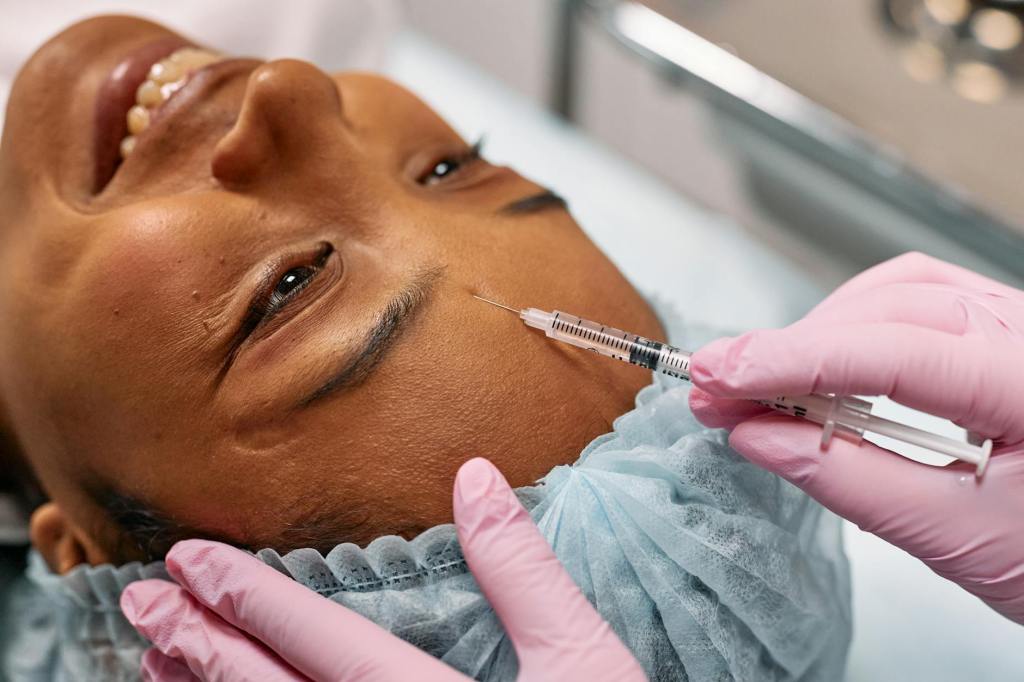
A small injection of strictness: The TGA’s clampdown on cosmetic injectables advertising
The Therapeutic Goods Administration (TGA) recently published updated guidance on advertising cosmetic injectables. It’s a reminder that advertising prescription drugs in Australia is prohibited. But what are the issues here?
-

The first pig kidney has been transplanted into a living person. But we’re still a long way from solving organ shortages
Reports are increasing of patients receiving xenotransplanted organs under ‘compassionate use’ exemptions. The number of CRISPR/Cas9 genome edits are also increasing. But the science does not yet demonstrate ‘proof of principle.’
-

Choosing a new doctor? Earlier sexual misconduct may soon be on the public record
Reports of sexual misconduct by Australian health practitioners against patients continue to increase. Now, Australian health ministers are considering three interesting amendments intended to protect patients from boundary violations.
-

Regulating harmful cross-border advertising: can it be done?
How do governments prevent their citizens from being exposed to harmful online advertising which originates outside of their jurisdiction? Such advertising is referred to as cross-border advertising. Advertisers have taken advantage of a digitised, interconnected world to reach broad audiences (including children) across national borders.
-

Alcohol causes 3 million deaths each year. Eliminating conflicts of interest is vital to bringing this number down
Alcohol causes three million deaths each year, including 13.5% of deaths amongst those aged 20-39 years. But the personal and economic costs of alcohol-related harm are not met by the alcohol industry.
-

Indigenous Peoples’ Inclusion in Food Governance
For NAIDOC Week, Dr Mark Lock speaks to Dr Belinda Reeve about championing health equity and inclusion for First Nations Australians in food governance.
-

Alcohol companies continue to play by their own rules, putting our children’s health at risk
Alcohol companies are largely left to write and administer their own rules through the Alcohol Beverages Advertising Code (ABAC) Scheme.
-

Another step forward for the Pacific Legislative Framework
Pacific Island Countries and Territories have some of the world’s highest rates of health risks. In response, the Public Health Division of the Pacific Community (SPC) has been driving an initiative for tackling the key risk factors: the Pacific Legislative Framework.
-

Closing the Gap and health governance reform: a brief review
The National Agreement on Closing the Gap is an ambitious all-of-government framework for improving the health and welfare of Australia’s first nations peoples. This post briefly reviews the Agreement and considers its significance as an example of health governance reform.
-
Big Alcohol and COVID-19: industry rules fail. Again.
By Hannah Pierce, Kathryn Backholer, Sarah Jackson and Florentine Martino Reposted from MJA Insights: https://insightplus.mja.com.au/2021/11/big-alcohol-and-covid-19-failing-self-regulation-again/ WE know some people are more likely to drink – and drink more – during times of uncertainty and stress. Unsurprisingly, the alcohol industry is also aware of this. The COVID-19 pandemic has illustrated how quickly and creatively the alcohol industry will…