Category: Healthcare Law
-
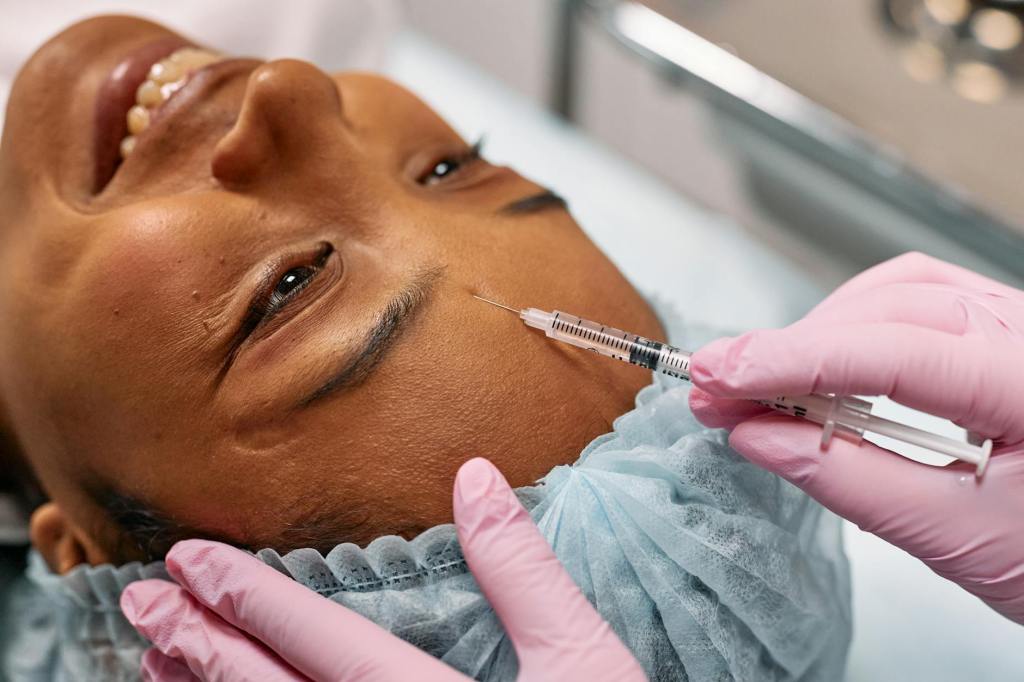
A small injection of strictness: The TGA’s clampdown on cosmetic injectables advertising
The Therapeutic Goods Administration (TGA) recently published updated guidance on advertising cosmetic injectables. It’s a reminder that advertising prescription drugs in Australia is prohibited. But what are the issues here?
-
![Case note: Fidge v Pfizer Australia Pty Ltd [2024] FCA 161](https://sydneyhealthlaw.files.wordpress.com/2024/03/pexels-photo-5863366.jpeg?w=867)
Case note: Fidge v Pfizer Australia Pty Ltd [2024] FCA 161
In a case interesting for many reasons, Rofe J of the Federal Court of Australia has held it is not an ‘incident of medical practice’ for medical practitioners to challenge alleged offences under law to (putatively) protect patients.
-

Choosing a new doctor? Earlier sexual misconduct may soon be on the public record
Reports of sexual misconduct by Australian health practitioners against patients continue to increase. Now, Australian health ministers are considering three interesting amendments intended to protect patients from boundary violations.
-

Let guidelines be your guide: AHPRA and National Boards to reform cosmetic procedures sector
As the guidelines develop, it will be interesting to see how the regulator and Boards attempt to deal with the difficult problem of social media promotion in this very popular sector.
-

Doctors may soon get official ‘endorsements’ to practise cosmetic surgery – but will that protect patients?
People who are interested in exploring whether cosmetic surgery is appropriate for them are right to feel wary and confused. Now, the introduction of a scheme to officially endorse doctors who practise in the area of cosmetic surgery promises to allay patients’ doubts. But the idea remains contentious for those in the field.
-

Thinking about cosmetic surgery? At last, some clarity on who can call themselves a surgeon
Currently, doctors doing cosmetic surgeries can call themselves ‘surgeons’ without special training. But soon, the title will be protected.
-

Who’s the best doctor for a tummy tuck or eyelid surgery? The latest review doesn’t actually say
If you’re thinking about cosmetic surgery, how do you know which health practitioner to trust? A review of how cosmetic surgery is regulated in Australia, released today, may help consumers decide.
-

Developed countries, dwindling national flexibilities, and access to essential medications during public-health emergencies
Developed countries have wound back the breadth and effectiveness of flexible obligations in international patent agreements.
-
The courts’ role in treatment for childhood gender dysphoria: recent updates
In 2020 and 2021, there were significant developments in the courts’ role in treatment for childhood gender dysphoria. The UK case of Bell v Tavistock is well known, but Re Imogen is of more practical importance here in Australia. Both cases illustrate the changing role of the courts in treatment for childhood gender dysphoria, following…
-

The Covidsafe app: speed at the expense of transparency and accountability
Australia’s COVIDSafe app was launched by the Australian Government in April 2020. But the app has been hampered by concerns about its security, privacy, and effectiveness.