Category: Healthcare ethics
-
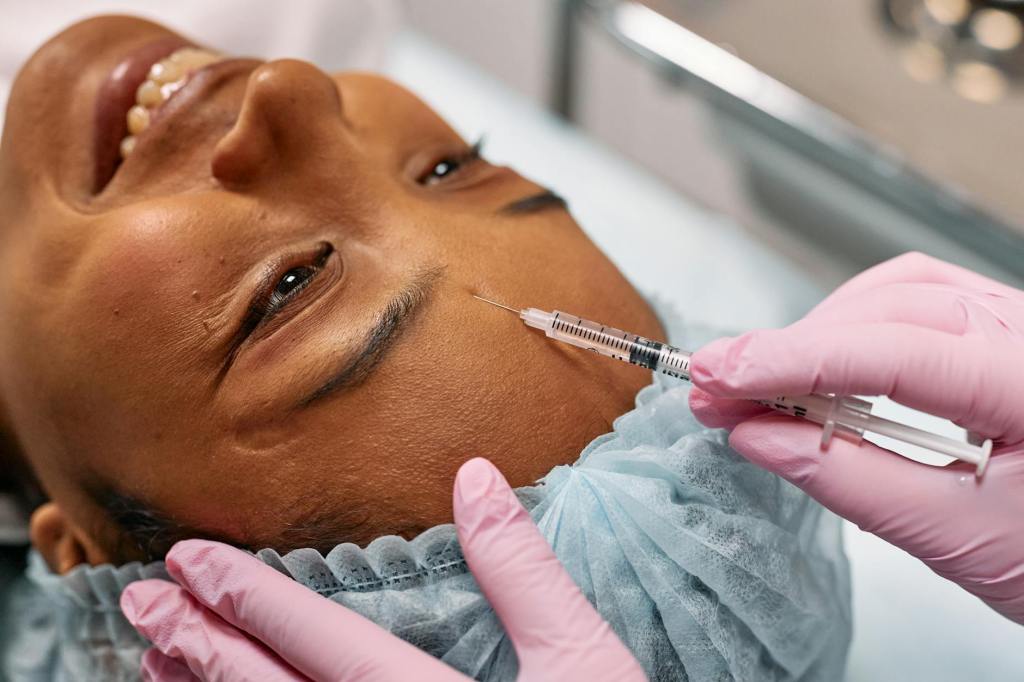
A small injection of strictness: The TGA’s clampdown on cosmetic injectables advertising
The Therapeutic Goods Administration (TGA) recently published updated guidance on advertising cosmetic injectables. It’s a reminder that advertising prescription drugs in Australia is prohibited. But what are the issues here?
-

The first pig kidney has been transplanted into a living person. But we’re still a long way from solving organ shortages
Reports are increasing of patients receiving xenotransplanted organs under ‘compassionate use’ exemptions. The number of CRISPR/Cas9 genome edits are also increasing. But the science does not yet demonstrate ‘proof of principle.’
-
![Case note: Fidge v Pfizer Australia Pty Ltd [2024] FCA 161](https://sydneyhealthlaw.files.wordpress.com/2024/03/pexels-photo-5863366.jpeg?w=867)
Case note: Fidge v Pfizer Australia Pty Ltd [2024] FCA 161
In a case interesting for many reasons, Rofe J of the Federal Court of Australia has held it is not an ‘incident of medical practice’ for medical practitioners to challenge alleged offences under law to (putatively) protect patients.
-

Doctors may soon get official ‘endorsements’ to practise cosmetic surgery – but will that protect patients?
People who are interested in exploring whether cosmetic surgery is appropriate for them are right to feel wary and confused. Now, the introduction of a scheme to officially endorse doctors who practise in the area of cosmetic surgery promises to allay patients’ doubts. But the idea remains contentious for those in the field.
-

Who’s the best doctor for a tummy tuck or eyelid surgery? The latest review doesn’t actually say
If you’re thinking about cosmetic surgery, how do you know which health practitioner to trust? A review of how cosmetic surgery is regulated in Australia, released today, may help consumers decide.
-
The courts’ role in treatment for childhood gender dysphoria: recent updates
In 2020 and 2021, there were significant developments in the courts’ role in treatment for childhood gender dysphoria. The UK case of Bell v Tavistock is well known, but Re Imogen is of more practical importance here in Australia. Both cases illustrate the changing role of the courts in treatment for childhood gender dysphoria, following…
-
Named reporting of HIV: A positive step for public health?
In Australia, doctors must notify public health authorities of new cases of HIV/AIDs. However, strict confidentiality requirements apply to the testing, treating and notification of HIV, protecting the identity of patients. As part of its review of the New South Wales Public Health Act 2010, the Department of Health is considering whether to remove these…
-
NBOT Annual Workshop – Call for Papers
Date: 10 March 2016 Venue: Sydney Law School, University of Sydney In March, the Network for Bodies, Organs and Tissues (NBOT) will host its annual multi-disciplinary workshop on bodies and tissues. The event provides a forum for discussions of moral, ethical and regulatory issues relating to the access and control of tissue. The Network welcomes papers that…