Author: rogermagnusson
-

Vaping law reform: Protecting the Pacific
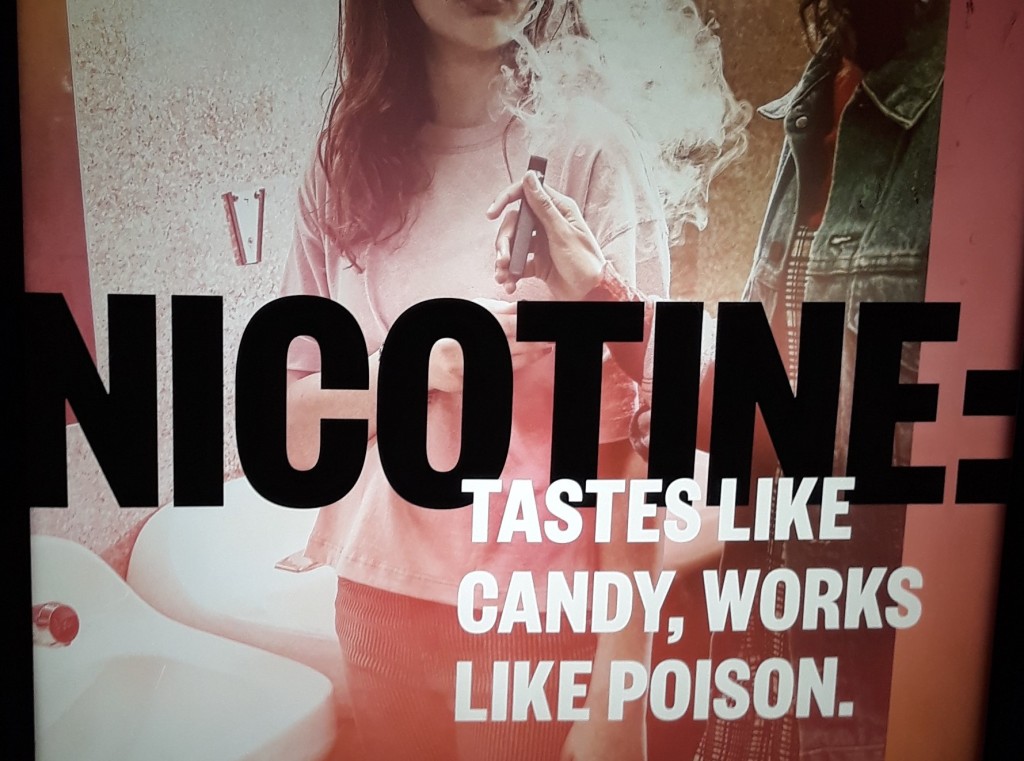
Vaping is on the rise and governments are scrambling to respond. Guest authors Sophia Bleakley, Clare Gim and Helen Zhang analyse the issues.
-

Strengthening Australia’s smoke and vape-free beach culture (north, and south, of the border)
Keeping beaches smoke and vape-free severs the link between relaxation and nicotine addiction. It says you don’t need to harm your body to enjoy yourself.
-
Vaping law reform: New South Wales in a federal context
There is a lot of vaping-related law reform activity going on in Australia at the moment. This (long) post reviews NSW vaping laws and provides a baseline for understanding the changes that are underway, both at NSW (State) and Commonwealth level. Background The failure to enforce nicotine control laws, together with ludicrously low penalties, have…
-

Proving the “competent professional practice” defence in NSW: Is the law any clearer after Dean v Pope?
Background A health practitioner who is sued for negligence in NSW will avoid liability under s 5O(1) of the Civil Liability Act 2002 (NSW) “if it is established that the professional acted in a manner that (at the time the service was provided) was widely accepted in Australia by peer professional opinion as competent professional…
-

Australia’s vaping train wreck: The Butler Plan to fix it and the devil in the detail
This post was written by Neil Francey, Research Affiliate, Sydney Health Law Australia’s Vaping Train Wreck Commonwealth Health Minister, Mark Butler MP, has announced that the Albanese Government is taking strong action to reduce smoking and stamp out vaping – particularly among young Australians – through stronger legislation, enforcement, education and support. This follows public…
-

Contraventions of the Australian Consumer Law in the promotion of e-cigarettes
This post was written by Neil Francey, Research Affiliate, Sydney Health Law In an article in The Conversation, “Sex and lies are used to sell vapes online. Even we were surprised at the marketing tactics we found”, published on 6 March 2023, Curtain University Professor Jonine Jancey notes that e-cigarettes are not harmless; they contain…
-

Pokies: joyless, nasty, and on the way out?
This post gives a shout out to hotel owners who are ditching their pokies to create a more family-friendly atmosphere. And to executives of registered clubs who are resisting pressure to make gambling the heart and sole of the business plan for registered clubs: see here and here. Let’s be honest: pokies (also known as…
-

Global health law short courses
If you live on planet earth, you have a stake in global health law. This post draws attention to two upcoming short courses taught by global health law colleagues in Europe. Summer in Geneva? The University of Geneva will be hosting a course on International Law, Global Health and Global Justice on June 26-30, 2023.…
-

Regulating harmful cross-border advertising: can it be done?
How do governments prevent their citizens from being exposed to harmful online advertising which originates outside of their jurisdiction? Such advertising is referred to as cross-border advertising. Advertisers have taken advantage of a digitised, interconnected world to reach broad audiences (including children) across national borders.
-

Alcohol causes 3 million deaths each year. Eliminating conflicts of interest is vital to bringing this number down
Alcohol causes three million deaths each year, including 13.5% of deaths amongst those aged 20-39 years. But the personal and economic costs of alcohol-related harm are not met by the alcohol industry.