Category: Uncategorized
-
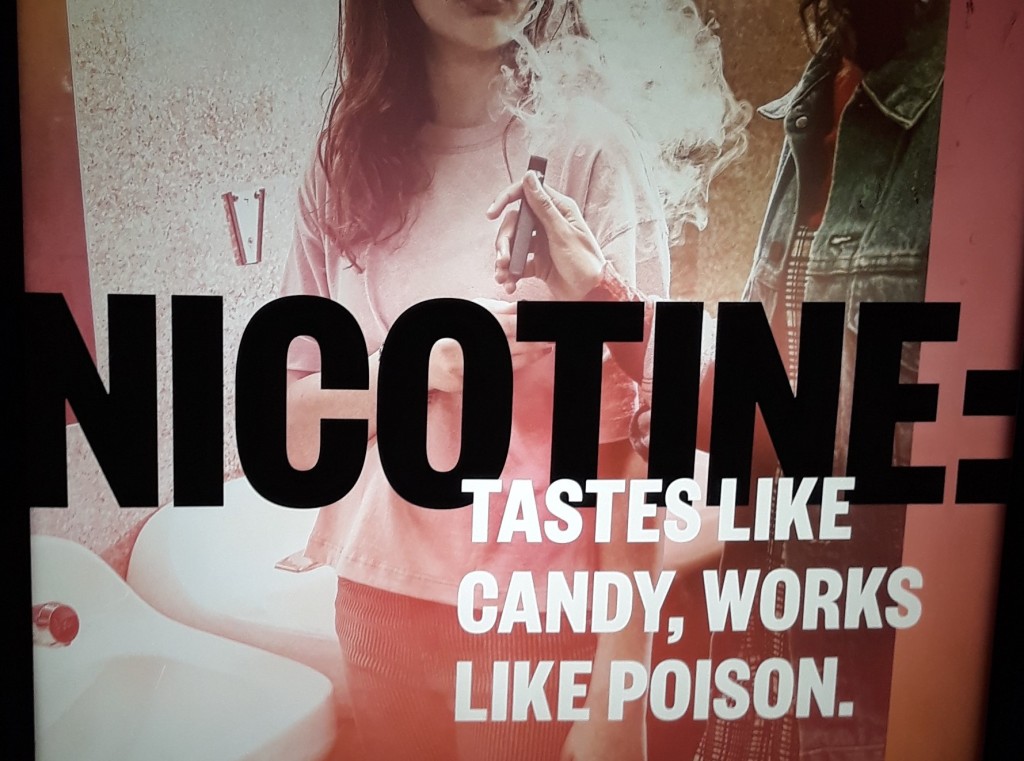
Vaping law reform: New South Wales in a federal context
There is a lot of vaping-related law reform activity going on in Australia at the moment. This (long) post reviews NSW vaping laws and provides a baseline for understanding the changes that are underway, both at NSW (State) and Commonwealth level. Background The failure to enforce nicotine control laws, together with ludicrously low penalties, have…
-

Proving the “competent professional practice” defence in NSW: Is the law any clearer after Dean v Pope?
Background A health practitioner who is sued for negligence in NSW will avoid liability under s 5O(1) of the Civil Liability Act 2002 (NSW) “if it is established that the professional acted in a manner that (at the time the service was provided) was widely accepted in Australia by peer professional opinion as competent professional…
-

Australia’s vaping train wreck: The Butler Plan to fix it and the devil in the detail
This post was written by Neil Francey, Research Affiliate, Sydney Health Law Australia’s Vaping Train Wreck Commonwealth Health Minister, Mark Butler MP, has announced that the Albanese Government is taking strong action to reduce smoking and stamp out vaping – particularly among young Australians – through stronger legislation, enforcement, education and support. This follows public…
-

Contraventions of the Australian Consumer Law in the promotion of e-cigarettes
This post was written by Neil Francey, Research Affiliate, Sydney Health Law In an article in The Conversation, “Sex and lies are used to sell vapes online. Even we were surprised at the marketing tactics we found”, published on 6 March 2023, Curtain University Professor Jonine Jancey notes that e-cigarettes are not harmless; they contain…
-

Global health law short courses
If you live on planet earth, you have a stake in global health law. This post draws attention to two upcoming short courses taught by global health law colleagues in Europe. Summer in Geneva? The University of Geneva will be hosting a course on International Law, Global Health and Global Justice on June 26-30, 2023.…
-
Vaccine mandates webinar
On 9 December, the Parsons Centre for Law & Business, together with Corrs Chambers Westgarth, convened a seminar entitled Vaccine mandates and public health orders: legal and ethical issues for business. The seminar reviews the emergence of vaccine mandates in public health orders in NSW, and vaccine mandates imposed by businesses and other organisations from…
-
A triumph for religious freedom, or viral spreading? The US Supreme Court in Roman Catholic Diocese of Brooklyn v Cuomo
During his Presidency, President Trump had the opportunity to appoint three new Justices to the U.S. Supreme Court. In 2017, the acerbic conservative Justice Neil Gorsuch replaced Justice Antonin Scalia; In 2018, Justice Brett Kavanaugh replaced retiring Justice Anthony Kennedy; and In 2020, Justice Amy Coney Barrett replaced Justice Ruth Bader Ginsburg. These three appointments…
-
The tricky business of Covid-19 reviews & origins investigations
Dr Dominic Dwyer, Australia’s member of the WHO-convened Global Study of the Origins of SARS-CoV-2, won’t remember me, but he was generous and helpful when I interviewed him as a PhD student in the early 1990s. His more recent comments to the media illustrate the challenges of attempting to investigate the origins of SARS-CoV-2 as…
-
Reckless, incompetent, outrageous: rogue doctors performing cosmetic surgery still a problem in NSW
A previous post briefly reviewed the regulation of cosmetic surgery in New South Wales. This post reviews the decision of the NSW Civil and Administrative Tribunal in Health Care Complaints Commission v Blackstock. Professional disciplinary complaints in NSW First, some background. In NSW, professional disciplinary complaints against a medical practitioner can be made on a…