Tag: World Health Organisation;
-
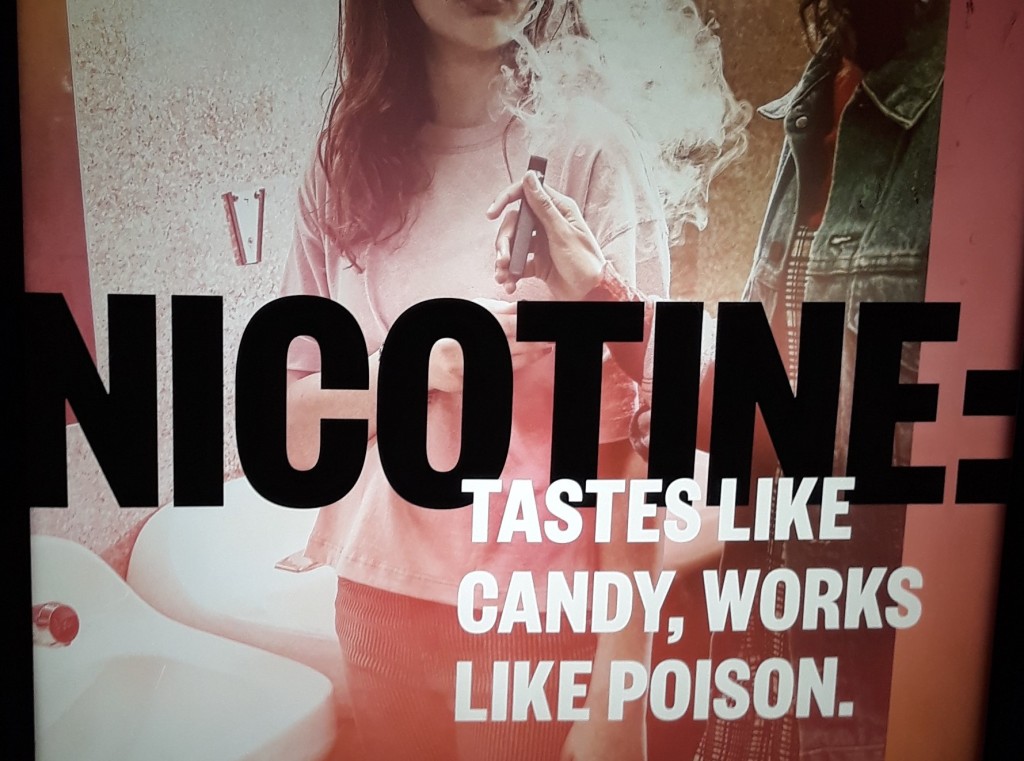
Vaping law reform: New South Wales in a federal context
There is a lot of vaping-related law reform activity going on in Australia at the moment. This (long) post reviews NSW vaping laws and provides a baseline for understanding the changes that are underway, both at NSW (State) and Commonwealth level. Background The failure to enforce nicotine control laws, together with ludicrously low penalties, have…
-

Regulating harmful cross-border advertising: can it be done?
How do governments prevent their citizens from being exposed to harmful online advertising which originates outside of their jurisdiction? Such advertising is referred to as cross-border advertising. Advertisers have taken advantage of a digitised, interconnected world to reach broad audiences (including children) across national borders.
-

Alcohol causes 3 million deaths each year. Eliminating conflicts of interest is vital to bringing this number down
Alcohol causes three million deaths each year, including 13.5% of deaths amongst those aged 20-39 years. But the personal and economic costs of alcohol-related harm are not met by the alcohol industry.
-

Another step forward for the Pacific Legislative Framework
Pacific Island Countries and Territories have some of the world’s highest rates of health risks. In response, the Public Health Division of the Pacific Community (SPC) has been driving an initiative for tackling the key risk factors: the Pacific Legislative Framework.
-

Prospects for the World Health Assembly’s pandemic instrument
The World Health Assembly (WHA) has established an intergovernmental negotiating body to “draft and negotiate a WHO convention, agreement or other international instrument on pandemic prevention, preparedness and response”. The Assembly’s decision was made at the special session of the WHA, convened for the specific purpose of considering the benefits of such an instrument. But…
-
The tricky business of Covid-19 reviews & origins investigations
Dr Dominic Dwyer, Australia’s member of the WHO-convened Global Study of the Origins of SARS-CoV-2, won’t remember me, but he was generous and helpful when I interviewed him as a PhD student in the early 1990s. His more recent comments to the media illustrate the challenges of attempting to investigate the origins of SARS-CoV-2 as…
-
Legal management of the novel Coronavirus (2019-nCoV) in Australia
On 31 January the Director-General of the World Health Organisation, Dr Tedros Adhanom Ghebreyesus declared the novel coronavirus (2019-nCoV) a public health emergency of international concern (PHEIC), following the advice of the Emergency Committee. (See here). Under the International Health Regulations, which govern global management of infectious disease outbreaks, a declaration that a PHEIC exists…
-
Australia and the language of fire
There are currently 100 fires burning across New South Wales. Fifty of them are uncontained, as the weather swings between baking hot, and blustery southerlies. Here in Sydney, the sky looks yellow. Soot is washing up on Sydney beaches, and clouds of dust are turning New Zealand glaciers pink. According to the Bureau of Meteorology…
-
International Guidelines on Human Rights, Healthy Diets and Sustainable Food Systems: could they make a difference?
The BMJ has published an Opinion calling on the Director-General of the World Health Organisation, Dr Tedros Adhanom Ghebreyesus, and the United Nations High Commissioner for Human Rights, Dr Michelle Bachelet, to jointly initiate a process to develop International Guidelines on Human Rights, Healthy Diets, and Sustainable Food Systems. 180 signatories from 38 countries have supported…
-
The World Health Organisation, the International Health Regulations, ebola and other pandemics: seminar announcement
The International Health Regulations (IHR) (2005) are the primary global instrument for responding to, and seeking to prevent and limit the impact of public health emergencies of international concern, including communicable diseases with pandemic potential. The International Health Regulations are legally binding on all World Health Organization (WHO) Member States, including Australia. The IHR were…