Tag: children
-
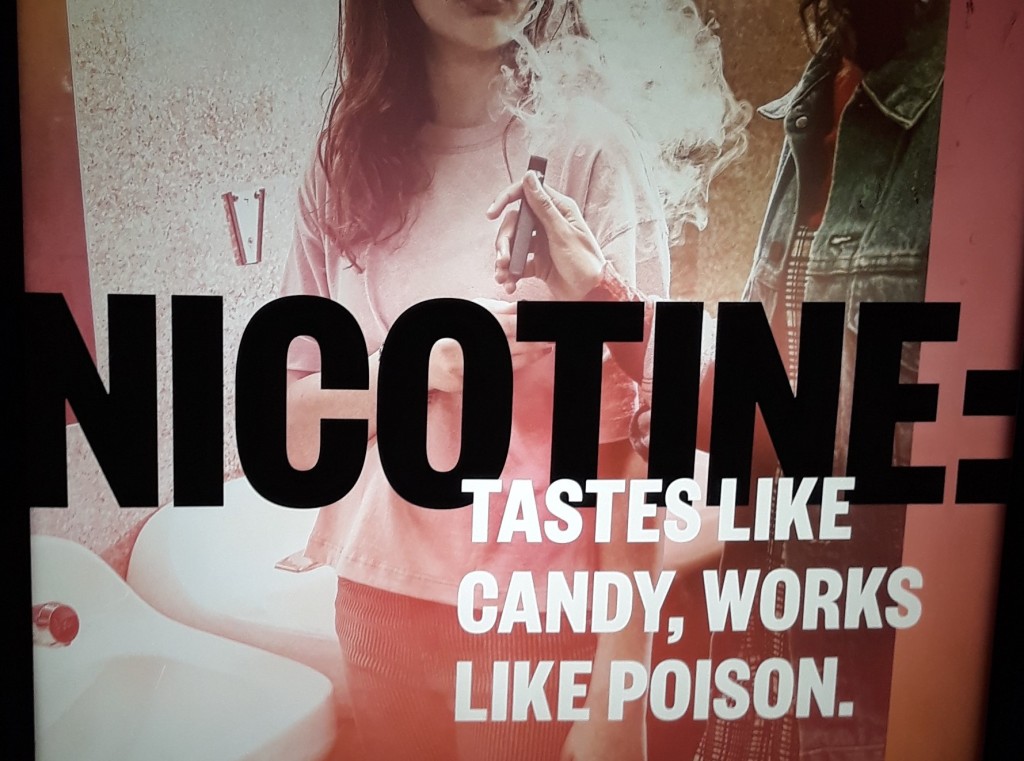
Vaping law reform: New South Wales in a federal context
There is a lot of vaping-related law reform activity going on in Australia at the moment. This (long) post reviews NSW vaping laws and provides a baseline for understanding the changes that are underway, both at NSW (State) and Commonwealth level. Background The failure to enforce nicotine control laws, together with ludicrously low penalties, have…
-
The courts’ role in treatment for childhood gender dysphoria: recent updates
In 2020 and 2021, there were significant developments in the courts’ role in treatment for childhood gender dysphoria. The UK case of Bell v Tavistock is well known, but Re Imogen is of more practical importance here in Australia. Both cases illustrate the changing role of the courts in treatment for childhood gender dysphoria, following…
-
Breastfeeding rooms in US federal buildings: who would have thought?!
Last year the US watered down a resolution of the World Health Assembly that would have called on States to “protect, promote and support breast-feeding”, and to provide technical support to “halt inappropriate promotion of foods for infants and young children”. A step too far, apparently, given the economic interests of US-domiciled formula companies. See…
-
Medical treatment in the best interests of the child: onshore, and offshore
There are troubling disparities between the medical treatment that children receive, depending on whether they live onshore – in Australia, or offshore – in immigration detention in places like Nauru. But do these disparities have a legal basis? Medical treatment and the best interests of the child: onshore Exercising their parens patriae jurisdiction, Australian Supreme…
-
The people’s award for undermining taxpayer-funded health promotion messages goes to…
(drum roll) The people’s award for undermining taxpayer-funded health promotion messages goes to… Mars Wrigley Confectionary, makes of Maltesers, a confectionary multinational who have just launched this Maltesers-inspired chocolate bar into Australia. You’ll want to sit down for this, it urges in billboard advertising. Clearly something momentous. A new chocolate bar. With Maltesers. Call…
-
Verifying IVF births involving donated sperm, eggs or embryos: changes to the law in New South Wales
A previous post discussed the case of Natalie Parker, an Australian mother of two young boys who, following the conclusion of IVF treatment, donated three spare embryos to a woman she met on the Embryo Donation Network, a place where donors and recipients can advertise and make contact. Parker was prepared to donate the embryos,…
-
Regulation of alcohol advertising is failing Australia’s young people: new research on the ABAC Code
Exposure to alcohol advertising influences the likelihood that young people will begin drinking, that those already drinking will increase their intake, or engage in risky drinking. Accordingly, the World Health Organization calls for regulation that reduces the impact of alcohol marketing on young people, including by addressing the content and volume of marketing, as well as…
-
Manslaughter by gross negligence, or systemic failure? Implications of the Dr Hadiza Bawa-Barba case for Australia
Sydney Law School and the Menzies Centre for Health Policy at the University of Sydney are co-hosting an evening seminar entitled “Manslaughter by gross negligence, or systemic failure? Implications of the Dr Hadiza Bawa-Garba case for Australia”. This event will be held at the Law School on Thurs 8 November, 6.00-7.30pm. You can register here.…
-
Upcoming events: Protecting children from unhealthy food marketing – learning from the past, ideas for the future
Along with Cancer Council NSW and the Charles Perkins Centre’s Food Governance Node, Sydney Health Law is hosting an event on regulation of unhealthy food marketing to children. Protecting children from unhealthy food marketing remains a hot topic, given increasing concern about children’s diet-related health. In Australia, food marketing to children is regulated largely through…
-
First, protect the child, then worry about the penitent sinner: South Australia’s new mandatory reporting legislation
South Australia is on a collision course with the Catholic Church hierarchy following passage of the Children and Young People (Safety) Act 2017. Chapter 5, Part 1 (ss 30-31), deals with reporting of suspicion that a child or young person may be at risk. These sections come into effect on 22 October 2018, and impose…