-
Navigating the ‘regulatory quagmire’ for extracellular vesicle therapies in Australia
Extracellular vesicles are generating excitement as tools for regenerative medicine and drug delivery — but no EV-based therapeutic has received market approval anywhere in the world. In a new Perspective article, we argue the barriers are not solely technical. They are also regulatory.
-
Innovation down under 2: tobacco endgame strategies in New Zealand (the UK & USA)
A recent post reviewed the tobacco control innovations introduced into Australia through the Public Health (Tobacco and Other Products) Act 2023 (Cth). New Zealand was legislating world-leading innovations of its own around the same time, although their purpose and design contrast sharply with tobacco control measures in Australia. If Australia’s legislation is best seen as…
-
Inaugural Carney Public Lecture | Australian Social Services Scandals: Towards dystopia? Or equity and justice for the vulnerable?
Thursday 11 December Time: 6-7.30pm (Refreshments to follow lecture)Venue: Law Lounge, Level 1, New Law Building Annexe (F10A)Eastern Avenue, University of Sydney, Camperdown campus Register for this free public lecture here In this lecture, Emeritus Professor Terry Carney explores the harm and injustices experienced by vulnerable Australians due to social services program failures such as Robodebt, employment services…
-
Rethinking Australia’s tobacco revenue plunge
This post was written by Neil Francey, Research Affiliate, Sydney Health Law In an article in The Weekend Australian (13-14 September 2025), Associate Editor Eric Johnston argues that there should be a rethink of tobacco customs and excise duty, due to the scale of illicit trade in tobacco. Johnston’s piece was prompted by burnt-out tobacco…
-
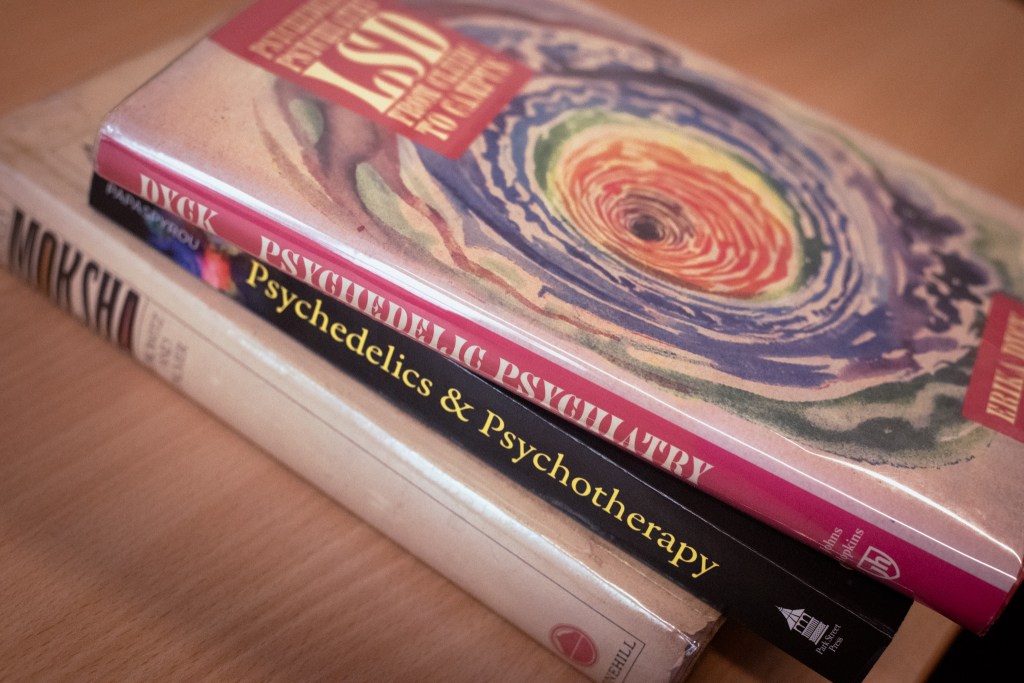
Two years on from Australia’s bold psychedelic experiment, here are our concerns
While a new Melbourne trial finds psilocybin-assisted therapy beneficial for the mental health of terminally ill patients, Australia’s broader experiment with medical psychedelics faces challenges. Our analysis raises concerns over a patchwork of regulations, unlawful promotion, and the potential for patient harm, and urging improvements to the authorised prescriber scheme.
-
Could a national tobacco retail licensing scheme help to combat illicit tobacco in Australia?
High tobacco excise has fueled a costly black market, creating what one economist calls a ‘dumb trifecta’ of crime, poorer health, and lost revenue. With inconsistent state laws seemingly failing, this post explores if a single, national tobacco retail licensing scheme could be a more effective solution.
-
Innovation down under 1: what has Australia been doing in tobacco control recently?
As discussed in another post, there has been so much vaping law reform in Australia over the past couple of years that it’s easy to overlook significant tobacco control law reforms. Since 2023, Australia has had a flagship, national tobacco control Act. The Public Health (Tobacco and Other Products) Act 2023 [PHTOP Act] consolidated previous…
-
Tracing Australia’s vaping controls back to source
The regulation of vaping and e-cigarettes in Australia underwent significant reform during 2023-2024. This post, prepared for health law students, traces some of the most significant reforms back to their legislative sources. Broad overview Australia’s regulatory framework for vaping has three components. First, vaping goods are regulated under the Therapeutic Goods Act 1989 (Cth), under…
-
Paradise at risk: recommendations to control tobacco and alcohol industry interference in Pacific Island Countries and Territories
This post was written by Matthew Catanzariti, Jessica Heaney and Oscar Loughnan Tobacco and alcohol represent significant threats to public health. The businesses that manufacture, distribute, and market these products to the public have irreconcilable interests to those that attempt to improve and protect public health. These businesses use coercive techniques, such as lobbying, tactical…
-
What is sexsomnia? And how can it be used as a defence in court?
Over the past decade, ‘sexsomnia’ has been used as a defence in a number of Australian sexual assault trials. But how can sexsomnia be proved in court? And what do we know about this rare condition?
-
Spill your guts, it could be good 4 u: Three ‘lessons’ doctors can learn from teenage girls
In Olivia Rodrigo’s sophomore album ‘Guts’ (2023), the pop artist centers the ‘messy emotions’ and mistakes she has made growing up. While Rodrigo’s fans have embraced this introspective approach, can medical practitioners learn anything from the process?
-
Teenagers refusing life-saving cancer treatment for religious reasons
Should courts allow minors (<18 years) to refuse life-saving medical treatment for religious reasons? My students don’t all agree that respect for the personal autonomy of a minor who fully understands the consequences of their decision, is all that matters. But many of them do.
-
How old’s too old to be a doctor? Why GPs and surgeons over 70 may need a health check to practise
Surging complaints against older doctors has prompted the Medical Board of Australia to propose reforms for this cohort. But haven’t we moved on from set retirement ages? And would this amount to discrimination?
-
Legislative restrictions on irreversible surgery on intersex children in the ACT: An unsurprising development?
Over a number of decades, personal autonomy has become a dominant value in Australian medical law. Yet, as new legislation restricting intersex interventions illustrates, the content of personal autonomy is subtly changing.
-
A small injection of strictness: The TGA’s clampdown on cosmetic injectables advertising
The Therapeutic Goods Administration (TGA) recently published updated guidance on advertising cosmetic injectables. It’s a reminder that advertising prescription drugs in Australia is prohibited. But what are the issues here?
-
The first pig kidney has been transplanted into a living person. But we’re still a long way from solving organ shortages
Reports are increasing of patients receiving xenotransplanted organs under ‘compassionate use’ exemptions. The number of CRISPR/Cas9 genome edits are also increasing. But the science does not yet demonstrate ‘proof of principle.’
-
Vaping law reform: Protecting the Pacific
Vaping is on the rise and governments are scrambling to respond. Guest authors Sophia Bleakley, Clare Gim and Helen Zhang analyse the issues.
-
Case note: Fidge v Pfizer Australia Pty Ltd [2024] FCA 161
In a case interesting for many reasons, Rofe J of the Federal Court of Australia has held it is not an ‘incident of medical practice’ for medical practitioners to challenge alleged offences under law to (putatively) protect patients.
-
Strengthening Australia’s smoke and vape-free beach culture (north, and south, of the border)
Keeping beaches smoke and vape-free severs the link between relaxation and nicotine addiction. It says you don’t need to harm your body to enjoy yourself.
-
Choosing a new doctor? Earlier sexual misconduct may soon be on the public record
Reports of sexual misconduct by Australian health practitioners against patients continue to increase. Now, Australian health ministers are considering three interesting amendments intended to protect patients from boundary violations.
A blog on health governance, law, and ethics, by health law experts at Sydney Law School
Contributors
Categories
- Forensic Criminal Law (1)
- Global Health (8)
- Health and technology (3)
- Health Policy (29)
- Health Profession Regulation (5)
- Healthcare ethics (10)
- Healthcare Law (25)
- Human Rights (4)
- Mental Health (5)
- postgraduate study (1)
- Public Health Law (34)
- Food (18)
- smoking (1)
- Uncategorized (92)
Tag cloud
advertising alcohol alcohol industry children Chronic disease prevention Covid-19 food policy Global Health health development Health Policy Human rights Non-communicable diseases (NCDs) obesity prevention public health law tobacco tobacco; e-cigarettes; nicotine tobacco industry World Health Organisation;
Latest comments
Nice piece Roger. Sam Egger’s recent paper on how the rise of vaping in NZ youth has slowed the decline…
“Clear the Air: Stronger Vaping Laws for a Healthier NSW” New South Wales (NSW) must take urgent action to align…
A blog on health governance, law, and ethics, by health law experts at Sydney Law School
Social Media
Where We Are
New Law School Building (F10)
University of Sydney
NSW 2050 Australia
Proudly Powered by WordPress















![Case note: Fidge v Pfizer Australia Pty Ltd [2024] FCA 161](https://sydneyhealthlaw.com/wp-content/uploads/2024/03/pexels-photo-5863366.jpeg?w=867)


Thanks for the link Simon, and reference to Egger et al. We have previously noted that daily vaping among 15-16…